What is GERD?
Do you suffer from impaired quality of life due to digestive disorders like Gastroesophageal reflux disease (GERD)? Have you tried all the medications but don’t seem to be really effective in treating your condition? Well, you may choose to improve your quality of life parameters by exploring the functional medicine approach.
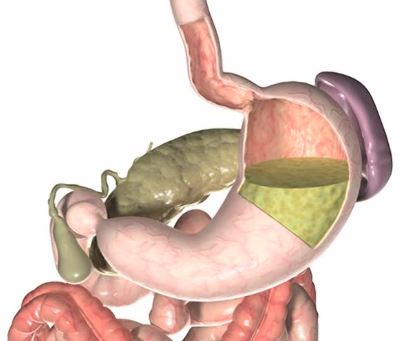
So, what is GERD really? GERD occurs when stomach acid often flows back into the tube connecting your mouth and stomach (esophagus). This backwash (acid reflux) can irritate the lining of your esophagus. Many people experience acid reflux from time to time. GERD is a moderate acid reflux that occurs at least twice per week, or moderate to severe acid reflux that occurs at least once weekly.
Most Individuals can handle the distress of GERD with lifestyle changes and over-the-counter drugs. However, some people with GERD may need stronger drugs or surgery to alleviate symptoms.
Over the past two decades, using Proton pump inhibitors (PPIs) has skyrocketed–combined with all the diagnoses of gastroesophageal reflux disease (GERD), amid growing concerns about improper prescriptions and possible adverse side effects. Now, a new study has linked the long-term use of those drugs to fatal cases of cardiovascular disease, chronic kidney disease, and upper gastrointestinal cancer. The cohort study, published May 30, 2019, from the journal BMJ, also discovered that such danger increases with the length of PPI use, even if the drugs are taken at low doses.
Taking an over-the-counter acid blocker for occasional heartburn symptoms might not be a huge problem, but in practice, many individuals with chronic reflux are prescribed acid blockers forever. But is this the best way to treat GERD? A substantial number of researchers, independently, have connected PPIs to adverse health problems such as bone fractures, chronic kidney disease, and pneumonia, among others.
GERD is A chronic, relapsing symptom which carries a risk of significant morbidity from causing complications. Numerous research suggests that individuals with GERD face impaired elements of quality of life like disturbed sleep, diminished energy, generalized body pain, disappointing sex life, and stress and have an effect on overall work productivity.
Given the risks associated with PPIs, What are a few options for treating the increasingly common issue of GERD? Medications that suppress symptoms might not be the best path.
How does Functional Medicine view GERD?
The Functional Medicine model is an Individualized, patient-centered, science-based approach that enables professionals and patients to work together to tackle the underlying causes of illness and promote optimal health. It requires a comprehensive understanding of each individual’s genetic, biochemical, and lifestyle variables and leverages that information to direct personalized treatment programs that result in improved patient outcomes.
The Functional Medicine frame can be particularly helpful for tapering from PPIs and to identify the underlying conditions of gastrointestinal issues (such as stress, sleep, or depression) and to develop and arrange individual therapy protocols with lifestyle, diet, nutraceuticals, pharmaceuticals, and botanicals, in addition to providing educational materials for patients to reevaluate their lifestyle treatments.
Rather than long-term pharmaceutical use, lifestyle modifications can help GERD patients find relief. Some that were analyzed for GERD include weight reduction, head-of-bed altitude, and avoidance of alcohol, tobacco, and late-night foods. Another modification that’s been indicated in the literature is avoiding foods that may aggravate reflux symptoms–e.g., caffeine, coffee, chocolate, spicy foods, highly acidic foods (oranges, tomatoes), and fatty foods. Recently, a prospective cohort study also found that smoking cessation significantly improved GERD symptoms in patients with normal body mass index and acute symptoms.
Functional Medicine treatment for GERD
Functional medicine for GERD is used to address the underlying causes of disease, through a system-oriented approach. The functional medicine model emphasizes food as the primary line of treatment and considers food as medicine that is essential for a healthy GI tract. A healthy gut is a critical foundation for health, and an evidence-based approach shows that many chronic complaints are linked to a compromised GI tract.
However, Functional nutritionists are trained to assess patients empirically, symptomatically, and in response to specific dietary interventions, lifestyle changes, and dietary supplements to treat the disease. Some of the important steps for functional medicine are mentioned below.
Betaine HCL
Supplementing your stomach with betaine HCL in GERD can promote the breaking down of dietary proteins helping in the prevention of food allergies associated with incomplete digestion of protein. Betaine HCL promotes gastric acid (HCL) secretion that is often suppressed by conventional treatments like PPI’S. Exogenous supply of Betaine HCL can play an important role in many physiological processes and thus aid in the treatment of GERD; it prevents the overgrowth of pathogens in the upper GI tract, promotes the absorption of essential minerals like calcium, magnesium, potassium, zinc, and iron and prepares folate and B12 for absorption.
Deal with Chronic stress
Stress can aggravate the symptoms of GERD. Research has shown that stress affects the nerves in your stomach, making it impossible to process the food properly. It depletes the production of prostaglandins in the stomach that is found to protect the stomach from acid. This leads to increased reflux. It’s very important to deal with your stress in order to digest your food properly. Breathing exercises performed before a meal can help digest your food better, along with certain lifestyle modifications like eating your meal at least 3 hours before going to bed.
Avoid sensitive food
Some foods can trigger reflux and it’s essential to avoid those foods in order to improve your quality of life as well as prevent yourself from worsening the GERD. Gluten and dairy are the most common ones, whereas others include Fried foods, Citrus foods, spicy foods, processed foods as well as avoid Alcohol, Caffeine, and Smoking. Medications such as aspirin, ibuprofen, naproxen can also aggravate GERD. All these foods can increase the reflux, and one can try avoiding them just for a few weeks and see the difference.
Supplement your gut- A healthy gut is a key to prevent many diseases including GERD. Supplements like probiotics and prebiotics are known to coat the stomach lining and help you digest your food. Similarly, digestive enzymes and various minerals like magnesium, zinc carnosine, calcium, and vitamins have been shown to help reflux. Herbal home remedies like aloe vera and licorice powder are taken before meals can help soothe your gut.
Some additional supplements for the healthy gut are mentioned below:
Magnesium
An evidence-based study has suggested that stress and GERD can deplete the levels of magnesium in the body. Magnesium is considered to be a very powerful relaxation mineral for the digestive system that is needed to relax the sphincter at the bottom of your stomach and helps prevent reflux by letting the food go down.
Melatonin
Melatonin has been found to have an important role in the regulation of sleep-wake cycles and circadian rhythms. Poor quality of sleep is one of the risk factors for GERD symptoms. It has also been found to possess mucosal protective effects where it protects gastrointestinal mucosa from oxidative damage caused by reactive oxygen species and by inhibiting gastric acid secretion. It is recommended to maintain a proper sleep cycle to prevent nocturnal symptoms such as night-time heartburn, improved quality of sleep and enhanced contractility of the lower esophageal sphincter.
Probiotics
GERD is often associated with Small intestinal bacterial overgrowth (SIBO) especially in patients who are under PPI’s therapy. SIBO is characterized by an elevated bacterial count that reflects changes in the composition and structure of the small intestine. SIBO presents with a variety of GI symptoms, such as abdominal distension, pain, diarrhea, and constipation. In such cases, probiotics that comprise of beneficial microorganisms can enhance the integrity of the intestinal mucosal barrier and balance the microbial ecosystem by inhibiting the growth of harmful bacteria. Probiotics are commonly administered to patients with intestinal flora abnormalities.
See: Functional Medicine For Heart Disease
Eliminate bad bacteria or yeast growing in your stomach
Some medications like antibiotics and hormone therapy can hamper the gut health and allow bad or harmful bacteria to grow in your gut. In fact, eating a lot of sugar and processed food can also contribute to bacterial overgrowth that can ferment the food and push things around and can cause reflux. It’s always good to avoid such foods and medication if you want to get relieved from GERD.
Research on Functional Medicine for GERD
1. First study: “Is It Useful to Administer Probiotics Together With Proton Pump Inhibitors in Children With Gastroesophageal Reflux?”
The aim of the study was to evaluate the prevalence of small intestinal bacterial overgrowth among children that received 12 weeks of PPI with or without probiotics. The study included 128 consecutive children suffering from GERD and a control group which included 120 healthy children. The GERD subjects were randomized into two groups
1. Placebo group (n= 64) received PPI and placebo treatment for 12 weeks and
2. Probiotics group (N=64) who received PPI and probiotics for 12 weeks.
After 12 weeks of treatment, Probiotics group showed a lower prevalence of dysbiosis concluding that probiotics administration decreased the rate of dysbiosis among children treated with PPI.
2) Second Study:
“Nutritional Interventions for Gastroesophageal Reflux, Irritable Bowel Syndrome, and Hypochlorhydria: A Case Report.”
43-year-old female suffering from anxiety, GI symptoms (dyspepsia, constant burping, abdominal pain, and constipation) and a recent diagnosis of small intestinal bacterial overgrowth (SIBO) was initially started on magnesium and digestive enzymes and was prescribed rifaximin 550 mg TID for 10 days. She reported an improvement in her constipation symptoms. However, her SIBO was not yet controlled and the treatment continued for another 4 months after which Her SIBO was controlled.
For her GI symptoms like anxiety, dyspepsia, gastritis, possible PPI-induced hypochlorhydria, and a diagnosis of IBS-C she was recommended with 75 mg zinc carnosine BID and 1 smoothie per day with added l-glutamine, slippery elm, GI repair powder, and low-allergenic pea protein powder. After 2 weeks most of her symptoms were controlled but her lower abdominal pain was still persistent for which she was recommended fiber like foods and aloe Vera juice. supplementation with hydrochloric acid (HCL)/betaine/pepsin was recommended for hypochlorhydria. After 2 months of treatment, she reported a complete resolution of the refractory lower abdominal pain with daily HCL supplementation.
Apart from all the above mentioned functional medicine approaches she was also advised on stress management and supplementing herself with probiotics.
Summary
A functional medicine approach is a system-oriented approach for treating GERD with multiple interventions. The combination of therapies like the implementation of a comprehensive functional nutrition approach that incorporated dietary guidelines, lifestyle recommendations, customized nutritional supplementation, and herbs can provide a successful outcome in conditions like GERD and associated symptoms like gastritis and hypochlorhydria.